The summer of 2013 was anything but normal for 10 year-old Zachary and his mom, Peggy. One day, Zach complained that his arm was tingling and “felt different.” Peggy took him to the local outpatient clinic. They didn’t know what to do about it and suggested she take him to the local emergency room. The doctor’s in the ER noticed Zach’s right shoulder was higher than the left. They did some checking and discovered a space between the bones. The doctor’s attributed this to growing pains. Zach and Peggy were sent home.
A couple of weeks later, Zach found a bump under his right arm and showed his mom.
“I had him lift his arm above his head, and I could see a tennis ball size bump under his arm. So we headed back to the doctor,” Peggy said. Their doctor sent them to a pediatric specialist. The pediatric specialist sent them to Massachusetts General Hospital. There, they performed a biopsy on the tumor and tested Zach’s bone marrow before diagnosing it as Ewing’s Sarcoma. Within a week after the diagnosis, Zach began in-patient chemotherapy for six days at a time, which Peggy said was grueling.
“Zach wasn’t eating, he experienced lots of side effects. The chemo made him feel like he was dying.” When the cycle was completed, his tumor had shrunk quite a bit, and the treatment was considered successful, even though some of it remained attached to a bone in his shoulder. In February 2014, Zach had surgery to remove what was left of the tumor. In order to do so, a big piece of his right scapula had to be removed as well. After surgery, Peggy was told that doctors were confident that Zach’s cancer had probably spread to other tissues in his body.
The next step was to try a different type of chemotherapy while undergoing six weeks of proton radiation. Zach completed this treatment in July of 2014 and was considered in remission.
One year later, during a routine CT scan of his chest, the doctors discovered a growth on Zach’s right lung. They told Peggy “we can’t just leave it. ” Zach began chemotherapy for the third time. After six weeks there was still no change. After testing to determine what types of treatment the tumor might respond to, the oncologist suggested a protein inhibitor. For the next four months, they tried it. It didn’t work. In fact, a CT scan showed the tumor had expanded, so treatment was stopped.
One of Zach’s doctors pointed them to a clinical trial in New Hampshire. At this point, Peggy was “tired, disappointed and frustrated” but willing to try just about anything that might help Zach. They were approved for the trial. However, it required surgery to extract cells to create a vaccine, as a form of immunotherapy. During surgery, additional tumors were discovered on Zach’s lung and diaphragm. They had to wait 4-6 weeks for the vaccine to be created, and then there was only a 50-50 chance Zach would get to try it, as the participants were divided into 2 groups. Zach was randomly chosen to be in the group that would be receiving chemo and not the vaccine.
“We opted out of the trial at that point, chemo had failed us so far, so I just didn’t think it would help. Plus, it was an eight hour drive each way, and that was just too much for Zach,” Peggy said. She has never found out if the vaccine was successful.
During all of this, Peggy and Zach began to feel isolated. The long drives back and forth to treatment didn’t leave much time for anything else, and Peggy feels the people in her community just didn’t know what to do or say, so they kept their distance. “I feel like we’ve been on a downhill slope for three years now,” she said. “You wish you could just wake up and it’s all gone – it’s pretty traumatic.”
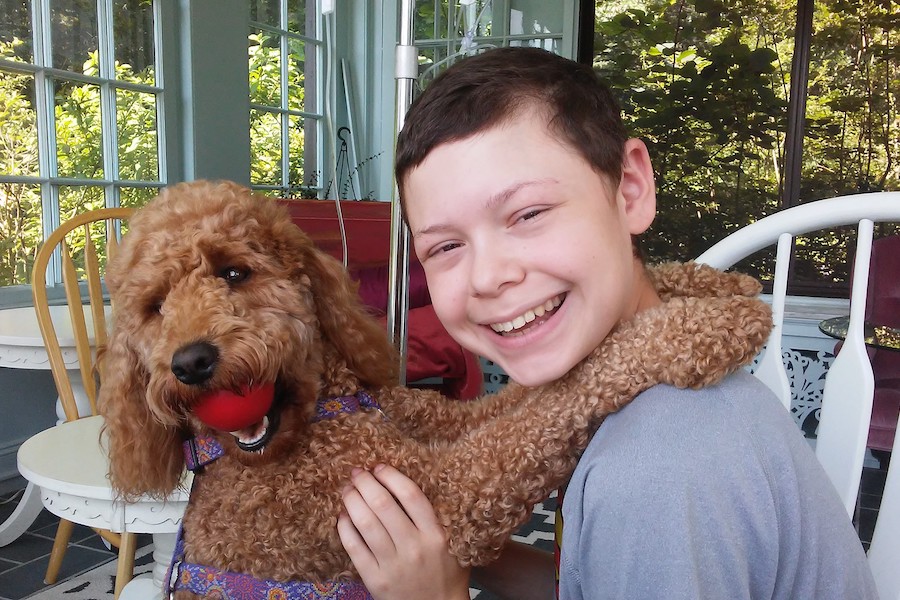
A couple of years ago, Peggy researched support animals and arranged to acquire a support dog for Zach, to alleviate the trauma he was feeling. Ginger, a golden-doodle, is a registered support dog, with an ID card and special vest, and has been traveling with them for over a year.
“Ginger is part golden retriever and part poodle. She can come to most oncology appointments. She travels well and stays in the hotel with us. She has been a blessing, as she reduces Zach’s anxiety,” said Peggy.
Peggy has now turned to an alternative therapy that seems to be having a positive effect on Zach. In March, Zach began high-dose vitamin C and alpha lipolic acid treatments via IV, twice a week, to continue for one year.
“Cancer likes glucose. This treatment is an antioxidant that is similar to glucose in structure. So, because it goes directly into the blood stream, the tumor should be attracted to it and take it in. It should kill the cancer cells,” Peggy explained. “So far, it seems to be working. At least, Zach looks and feels a lot better. We feel it’s boosting his immune system.”
But, the 372-mile round trip twice a week was costing Peggy over $400 per week and beginning to take a toll on her bank account. She suddenly remembered a bunch of pamphlets her social worker had given her that she hadn’t had time to look at. One of the brochures was for Compass to Care. After applying for assistance, Zach and his mom were quickly approved for support to get Zach to the hospital in Maine for his treatments.
“We are forever grateful for Compass to Care’s assistance. Without you, we would get discouraged. It lifts our spirits and gives us a reason to keep going, just knowing that there are people willing to support families going through cancer. It alleviates a lot of stress and anxiety, for both of us. It allows my focus to be on my child,” Peggy said.